Design, Analyze, Communicate: Working together to improve clinical study outcomes.
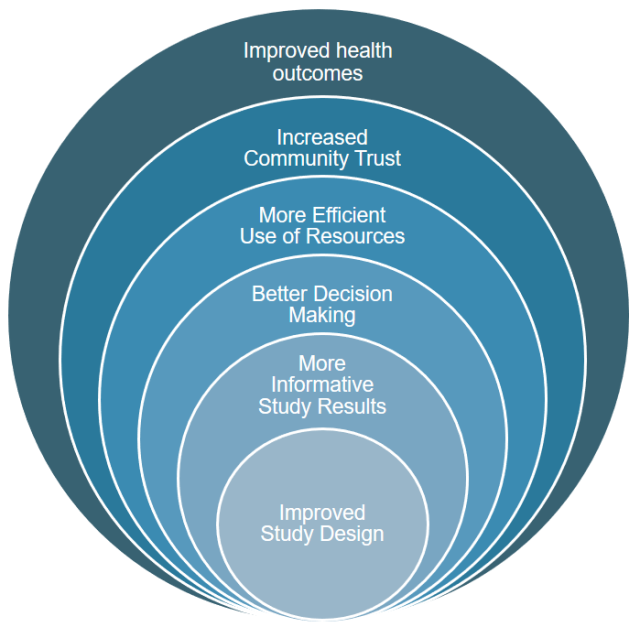
Creating informative clinical studies
Unfortunately, it is well documented that not all clinical studies provide robust answers to the questions being posed. In 2019, Deborah Zarin and colleagues coined the term “uninformative trials.”[2] “An uninformative trial is one that provides results that are not of meaningful use for a patient, clinician, researcher, or policymaker,” they wrote. In the supplement to their paper in JAMA, they identified 12 qualities of clinical trials associated with uninformative trials, which they called “red flags.” A year earlier, Professor Trudie Lang’s Global Health Network surveyed LMIC-based researchers about the parts of trials with which they needed methodological help.[3] Respondents coalesced around 27 factors. Other experts have published studies and guidance to address the same question.[4,5,6,7]
Creating informative clinical studies requires a team of qualified specialists. Frequently this includes but is not limited to principal investigators, experts in the given disease, pharmacologists, pharmacometricians (where the intervention is a drug or requires a dose and regimen selection), statisticians and operational experts. Many studies supporting advances in healthcare in LMICs also require local input.
Informativeness: what makes a trial “informative”?
An informative trial is designed to have the best chance to complete on time, answer its research questions definitively, and effect policy change or a go/no-go decision, by means of:
- locating trial sites based on epidemiology and impact rather than convenience,
- completing a statistical analysis plan concurrently with the trial protocol,
- using accepted endpoints and conservative effect and prevalence/incidence estimates, and
- utilizing contemporary techniques, such as statistical simulation, innovative trial designs, and software to monitor recruitment.”
Please note: Implementors of studies should also always refer to relevant regulatory standards and guidelines (e.g. FDA, EMA) to assist with study/protocol design.